By et al.
Source Sciencedirect
MAIT cells are known to have antimicrobial and antiviral properties, so it’s possible they could help limit the spread of the virus or reduce the severity of the illness.
Researchers now think the activation and movement of MAIT cells is triggered indirectly through signals from other immune cells and molecules. This shows MAIT cells are important in the body’s response to the COVID-19 virus, but they are not directly targeted by the virus.
Abstract
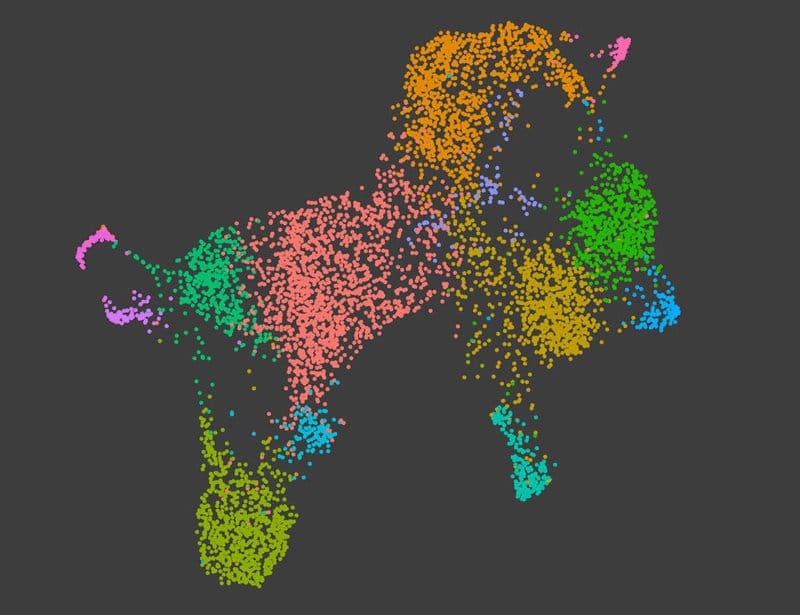
Prolonged T cell lymphopenia is common in COVID-19, caused by SARS-CoV-2. While the mechanisms of lymphopenia during COVID-19 remain elusive, it is especially pronounced in a specialized innate-like T cell population called Mucosal Associated Invariant T cells (MAITs). MAITs has been suggested to express Angiotensin-Converting Enzyme 2 (ACE2), which is the well-known cellular receptor for SARS-CoV-2. However, it is still unclear if SARS-CoV-2 can infect or affect MAIT cells directly. In this study, we performed multicolor flow cytometry on peripheral blood mononuclear cells obtained from COVID-19 patients to assess the frequencies of CD8+Vα7.2+CD161+ MAIT subsets at acute and convalescent disease phases. The susceptibility of MAITs and T cells to direct exposure by SARS-CoV-2 was analysed using cells isolated from healthy donor buffy coats by viability assays, virus-specific RT-PCR, and flow cytometry. In situ lung immunofluorescence was used to evaluate retention of T cells, especially MAIT cells, in lung tissues during acute COVID-19. Our study confirms previous reports indicating that circulating MAITs are activated, and their frequency is declined in patients with acute SARS-CoV-2 infection, whereas an accumulation of MAITs and T cells was seen in the lung tissue of individuals with fatal COVID-19. However, despite a fraction of MAITs found to express ACE2, no evidence for the susceptibility of MAITs for direct infection or activation by SARS-CoV-2 particles was observed. Thus, their activation and decline in the circulation is most likely explained by indirect mechanisms involving other immune cells and cytokine-induced pro-inflammatory environment but not by direct exposure to viral particles at the infection site.
Read more click here