Three weeks ago, Washington, D.C., resident Rebecca Read Medrano started feeling unwell. She had a dry cough, fatigue, nausea and terrible stomach pains that had her bending over.
There was one more symptom, and it was a bit odd. Medrano had largely lost her sense of taste. “My cousin was cooking, and everything he made tasted weird,” she recalls.
Medrano, 71, felt bad enough to go to her doctor for various tests, including testing for the coronavirus. Though she didn’t have a fever — considered a classic symptom of COVID-19 — she was concerned because her husband has a medical condition that puts him at higher risk of infection.
Last Saturday night, the results came back: She was positive.
Medrano’s case may not be just a fluke.
Doctors from Italy to China to South Korea to the U.S. are reporting cases where a loss of the sense of taste and the sense of smell, in particular, has been seen in patients who later tested positive for the coronavirus.
“The reason why the alarm bells were going off is that we’re all starting to see this, especially in parts of the United States with the most cases of COVID-19,” says Dr. Rachel Kaye, an assistant professor of otolaryngology at Rutgers University. Otolaryngologists specialize in head and neck surgery.
Reports are appearing on social media, including from celebrities who have tested positive for the coronavirus, such as Utah Jazz basketball player Rudy Gobert and American fashion blogger Arielle Charnas, weighing in on the “loss of smell” question. Both said they lost their sense of smell and taste.
So the question is, if you’ve lost your sense of smell and taste, is it possible you have the coronavirus — and should you try to get tested?
Globally, loss of sense of smell and loss of sense of taste are not considered symptoms of COVID-19 and are not part of the recommended screening criteria to be tested. Primary symptoms listed by the U.S. Centers for Disease Control and Prevention are familiar at this point: fever, cough and shortness of breath. The World Health Organization lists fever, tiredness and dry cough and includes shortness of breath on a list of “other” symptoms such as aches and pains, sore throat, diarrhea, nausea and a runny nose.
It is possible that the recent surge of media coverage of the “loss of smell and taste” story has prompted people to believe they’re experiencing such symptoms.
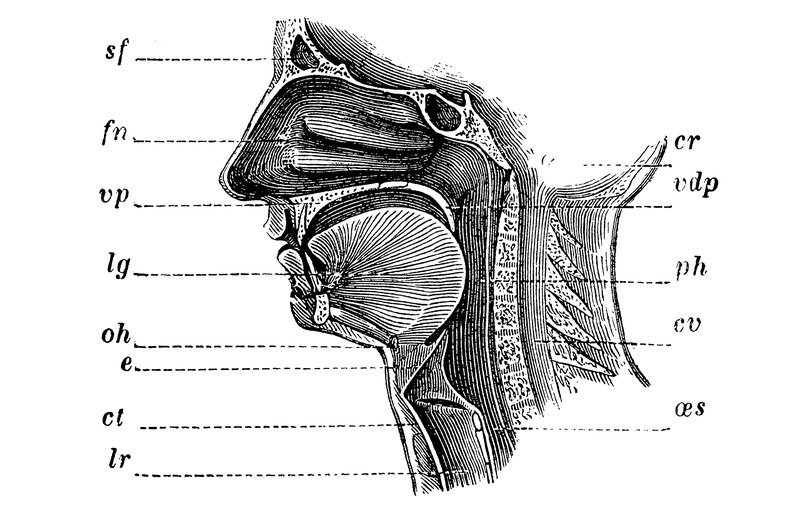
Then again, SARS-CoV-2 (the official name of the new coronavirus) may be able to infect the upper respiratory tract, which is home to the nose and nasal passages.
If anosmia and distorted sense of taste (dysgeusia) are indeed linked with COVID-19, that’s a possible clue that the coronavirus could be causing a range of upper respiratory issues. (And if you’re wondering why both senses might be affected, it’s because our sense of taste is largely driven by our sense of smell; those two senses are neurologically intertwined.)
That’s why ear, nose and throat doctors want to figure out: Is this a symptom of COVID-19?
“Everything tastes like cardboard”
For Kaye, the otolaryngology professor, the anecdotal evidence came to her doorstep. She saw a swell of patients reporting that their sense of smell and taste had suddenly vanished.
“I got a lot of, ‘Everything tastes like cardboard’ and ‘I can’t smell anything,’ ” Kaye said, speaking to NPR on Tuesday. Those patients did not demonstrate any of the other commonly cited COVID-19 symptoms.
But in the span of a week and a half, a number of them tested positive for the coronavirus — or were living with someone who was confirmed positive. And she heard about two dozen stories from fellow doctors saying similar things.
For Kaye, this raised the possibility that there was a whole host of other symptoms — beyond fever, cough and shortness of breath — that doctors and public health officials were overlooking in tracing the spread of this coronavirus.
“Obviously, people who are very symptomatic should be treated and confined to quarantine,” she says. “But the way to ‘flatten the curve’ is finding all these asymptomatic people and mildly symptomatic people. They’re the ice underneath the water of the iceberg. The danger is that these people unbeknownst to themselves are transmitting the virus.”
But there was a problem. Kaye had no way to statistically measure anosmia across a broad sample size of patients — to suss out confirmed cases of COVID-19 among those who had lost their sense of smell or taste. So she called the American Academy of Otolaryngology-Head and Neck Surgery and spoke to its leader, Dr. James Denneny, to suggest a possible survey of other doctors.
He told Kaye that his phone had been ringing with stories from ear, nose and throat doctors too.
“I had five or six different practices, different physicians, call me,” Denneny says. “They let me know that they were seeing anosmia — or lack of smell — or hyposmia — a decreased sense of smell — in patients for no reason, that then were tested positive for the coronavirus,” Denneny told NPR on Monday.
On Sunday, the American Academy of Otolaryngology published a statement proposing that anosmia, hyposmia and dysgeusia be added to the list of screening tools for COVID-19.
The goal is to alert doctors to the possible connection between these symptoms and COVID-19 and to suggest that those patients be tested for the coronavirus after determining that allergies and other infections aren’t to blame.
The organization is also strongly encouraging ear, nose and throat doctors to wear personal protective equipment when performing upper airway procedures and examinations, just in case a patient has COVID-19 and is asymptomatic or showing mild symptoms.
There is evolving evidence from China, Italy and Iran that otolaryngologists are among the highest-risk groups for contracting the virus.
It was a precautionary move by the American Academy of Otolaryngology, given the current lack of published research on how exactly SARS-CoV-2 disrupts the sense of smell — and now it’s trying to get a better picture of what doctors are seeing.
“Anything we can do to flatten this curve is critical”
As doctors consider this phenomenon, they are looking for explanations. The inflammation of the nasal passages caused by viral infection can lead to congestion — and that can inhibit the sense of smell, Kaye says.
Post-viral infection is a common cause for loss of smell in adults. “Any sort of upper respiratory illness can cause inflammation of the lining of the nasal passages,” Kaye says. “And when the nasal passages get swollen, it can lead to congestion.”
What’s more, says Kaye, it’s common for viral infections to limit airflow through the nose.
“Airflow is very important to distribute the smell molecules to the receptors in the nose. So there is a functional, anatomic structural issue that can happen with nasal congestion that can explain a loss of sense of smell,” Kaye says.
Kaye says there’s another possible explanation for a loss of sense of smell and taste.
“The thought is that there’s actually virally induced damage to the nerves or the nervous system that is producing that sense of smell,” Kaye says. “And we know that viruses can damage nerves in general.”
Denneny agrees. He says that nerve endings that sit on the lining of the nose, which transmit information to your brain on what you’re smelling, can be impacted by viruses.
“When the viral inflammation takes place, just like with any other virus, it can damage the nerve endings and decrease the ability to transmit what the particles are telling the nose, sending the message to the brain that ‘it is a flower’ or ‘it is a fire.’ So there’s no transmission,” Denneny says.
But at this moment, the exact mechanism for how SARS-CoV-2 might affect smell is still a mystery.
Yet Denneny didn’t want to wait for research to catch up before sounding the alarm. In talking to colleagues on the front lines of fighting this coronavirus, from Seattle to New York City, he decided to speak out in the interest of potentially saving lives — alerting doctors to be on the lookout for patients who have lost their sense of smell and taste, if those prove to be symptoms of COVID-19.
From there, doctors can recommend taking the appropriate precautions, such as staying at home and going into self-quarantine.
“Under the worst scenarios, someone’s isolated and it hasn’t hurt them,” Denneny says. “Under a disease-control scenario, it may prevent them from spreading it or otherwise propagating the disease. If you make an error, you’d rather err on being too conservative at this point.”
When asked if he hesitated in speaking publicly, Denneny gave a decisive “no.”
“Anything we can do to flatten this curve is critical. If it turns out not to be helpful, it won’t be damaging. It’s not like you’re getting a surgical procedure and taking a medicine you don’t need,” Denneny says. “If we’re able to identify something that helps flatten the curve even by 10 percent, it’ll be hugely valuable to this country or to other countries as well.”
Additionally, the American Academy of Otolaryngology has acted on its intent to survey clinicians on the association between loss of smell and cases of COVID-19. On Thursday, it made public a reporting tool to survey doctors around the world, inviting them to share what they’re seeing in patients.
“Are there more cases of anosmia than normal? And are these cases COVID-19 positive?” asks Kaye, who helped design the survey. In compiling anecdotal evidence, the American Academy of Otolaryngology hopes to come to its own conclusions about the link between smell and COVID-19.
Once the survey is complete, Denneny plans to submit the results to a peer-reviewed academic journal.
If the study concludes there is a link, Denneny wants to see federal policy changes. “One of the things we’re hoping to do in compiling these cases is to ask the CDC if it’s worth including [loss of smell] as a symptom. That’s one of the hopes,” says Denneny. “It would be up to them to make that determination.”
NPR reached out to the CDC for comment on the symptoms of COVID-19 and loss of smell but did not receive a reply by press time.
“It’s kind of a slippery virus”
Fortunately, Medrano, the Washington, D.C.-based patient, was able to be tested.
Her case seems relatively mild. While she still has that dry cough, she is slowly feeling better, and her sense of taste is starting to return. “It’s kind of a slippery virus, because one day you’re fine, next day you don’t feel so good. Then you feel fine. It’s been up and down,” says Medrano.
But without a test, those individuals losing their sense of smell or taste are left to wonder.
In London, Natalie Miller is in that gray area. For two days last week, Miller, 26, had been battling tiredness and a headache along with diarrhea. While cooking dinner with her husband on Friday, she burned the potato pancakes “without realizing.”
She took a few bites but tasted nothing. She added sauce and feta cheese to the pancakes to boost their flavor. Another bite. No taste. While Miller’s other symptoms have disappeared, her sense of taste has not come back.
Miller later learned that the colleague of someone she dined with two weeks ago tested positive for COVID-19. She has been in self-quarantine ever since, and the loss of smell and taste was her first clue that something wasn’t right.
“I definitely want to be tested,” Miller said, speaking to NPR on Tuesday. “I can’t imagine what else it could be. I could have written it off as a weird hangover or a weird cold. But to have it with no congestion, it’s just such a strange phenomenon,” she said.
Kaye, for her part, wishes testing were widespread in the United States, to capture all the ways COVID-19 is showing up in patients.
“In an ideal world, everyone across the nation would be tested,” she says. “Everyone across the nation would put in all their symptoms. And we would have a wonderful, well-designed study on what the actual symptoms are.”
類型: 文章
作者: Emily Kwong et al.
出處: npr
連結: https://www.npr.org/sections/goatsandsoda/2020/03/26/821582951/is-loss-of-smell-and-taste-a-symptom-of-covid-19-doctors-want-to-find-out